Reimagining Physician Compensation Models for a Resilient Future
A publication jointly authored by the lawyers of Jones Day and The BDO Center for Healthcare Excellence & Innovation
Executive Summary
The COVID-19 pandemic has raised concern among healthcare leaders about the preparedness of acute care systems to adapt to and manage large-scale environmental disruptions. Current physician compensation models do not align incentives with the dynamic and unique strategic priorities of health systems, especially in the face of unforeseen circumstances.
Advancements in the healthcare landscape have accelerated in the last decade, and hospitals have been slow to respond. Value-based care has become the new normal, but organizations are still reconciling how to compensate physicians for their delivery of quality care that leads to patient satisfaction and positive health outcomes. Amid the pandemic, providers have hastily adopted more forms of telehealth to continue operations, further highlighting the need for a physician compensation structure that encourages experimentation with new technology.
Our novel Contribution-Based Incentive (CBI) Model is established on measurable variable incentives that balance (1) productivity, (2) quality and (3) citizenship. The CBI Model pairs stabilizing base salary with customizable core incentives in a point-system, offering greater career autonomy to physicians. Customizable pay levers motivate providers based on their productivity, quality outcomes, organizational stewardship, and degree of clinical and extracurricular engagement.
By allowing for different combinations and weights of the three core incentives, systems can align compensation with the individual needs of their physicians and the overall strategic priorities of the organization to fundamentally reshape the physician-hospital relationship.
Introduction
Disruptions caused by the recent COVID-19 pandemic will have profound and long-lasting effects on the operations, and in some cases survival, of healthcare systems. Ramifications will extend to every level of these organizations, including hospital-physician relationships.
As acute-care systems grapple with financial, supply, and staffing constraints, they will need to rethink their physician compensation structures to meet both immediate and long-term needs. No organization is immune to these discussions, and physician compensation models are not a one-size-fits-all solution.
Traditional compensation models tied to fixed compensation, accumulated work relative value units (“wRVUs”), or rote allocations of revenues and expenses, failed to account for the surge in demand for virtual services and coordinated community care. As a result, the current model destabilized the physician workforce. Health systems need a novel approach to build a compensation framework for their providers for long-term sustainability, one that aligns with systemic efforts to pay for quality and outcomes in a consumer-centric system, rather than units of service.
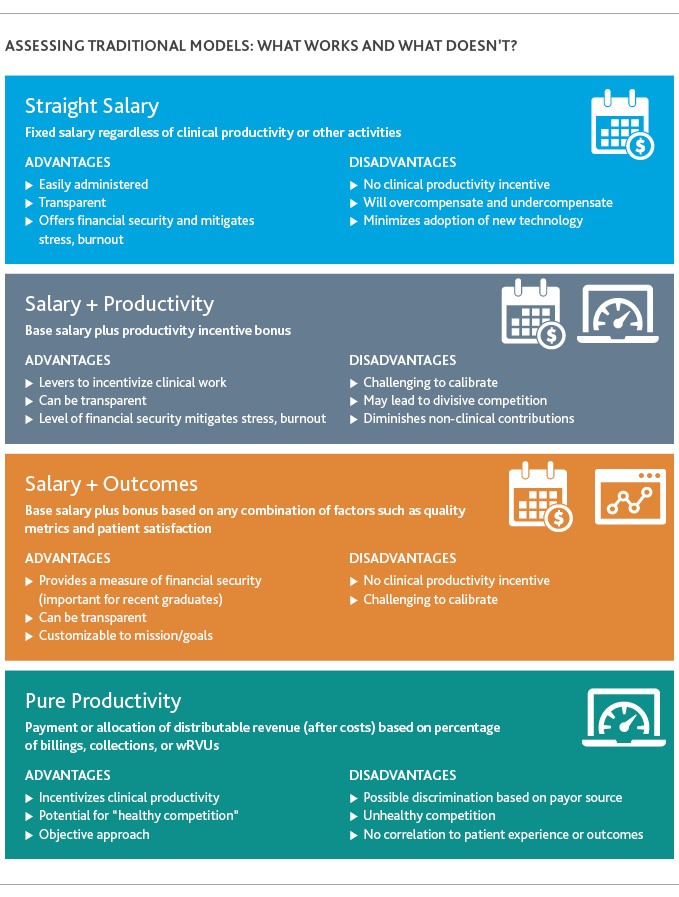
Before exploring opportunities to innovate, several common traditional physician compensation models are briefly summarized in the graphics on this page.
Rethinking the status quo: A New Contribution-Based Incentive Model (“CBI”)
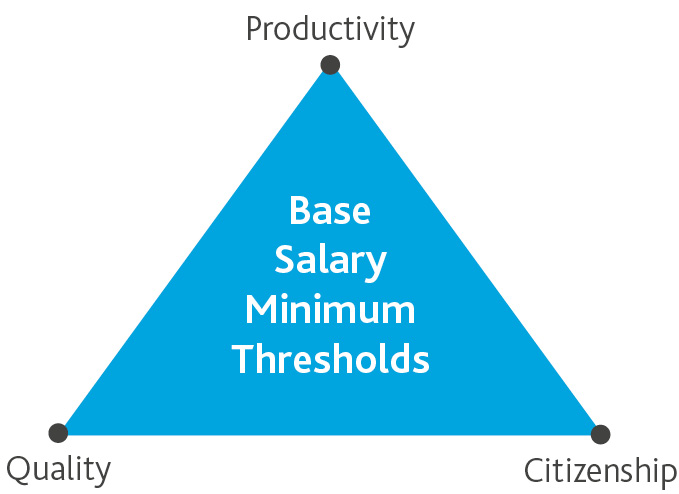
This paper proposes a new physician compensation model focused on measurable variable incentives that balance productivity, quality and citizenship. The CBI Model pairs stabilizing base compensation with customizable core incentives in a points-based, flexible system that offers greater career autonomy to the physician.
A flexible formula aligns disparate interests
The post-pandemic healthcare environment will further popularize salary-based compensation models as physicians seek more consistent and predictable pay. In this model, base salary is intended to be a modest but important component of overall compensation. While base salary might comprise a greater share of a recent graduate’s pay, physicians will have the opportunity to increase compensation through personal and team performance measured against variable metrics aligned with the organization’s mission, strategic direction, and specific goals.
Guaranteeing a modest base salary offers stability and mitigates risk of physician burnout or counter-productive financial stress. Transparency in the allocation of incentive points will motivate enhanced performance.
To be eligible for the bonus structure, physicians must satisfy baseline conditions of employment, including (1) regular clinical activity and associated productivity consistent with the range associated (on a fair market value basis) with the physician’s base compensation, (2) quality thresholds with outcome measurements set by the organization and (3) agreed upon citizenship efforts.
Physician behavior can be influenced by differentiating funding of each “Core Incentive” based on the organization’s mission, needs, and objectives, thereby incentivizing desirable activity using increased compensation potential.
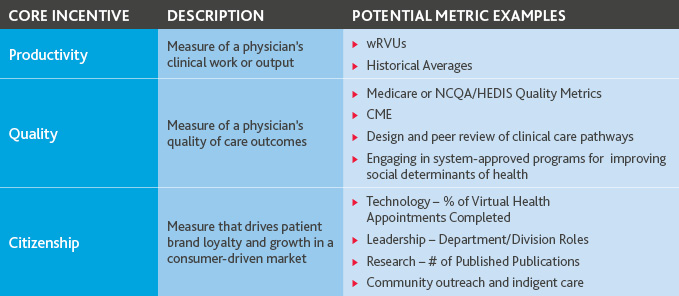
The fundamentals of the three core incentives
Productivity drives revenue
The prevailing standard for measuring physician productivity is work relative value units (“wRVUs”). Productivity-based incentive compensation may be paid based on ranges and is capped at reasonable levels (e.g., an appropriate percentage of base compensation, incentive compensative, or compensation benchmarks) based on specialty to guard against anti-cooperative behavior and incentives to over-utilize.
Quality measures put patients first
Both commercial and government payors have set standards for reimbursing providers based on quality. Providers are typically evaluated on metrics such as documented diagnosis on record, communication with the patient, intent to treat, pain control/symptom control, readmissions, and preventative screening measurements.
These reimbursement metrics help serve as minimum thresholds for quality outcomes but should be adapted based on a provider’s specialty, as well as clinical and non-clinical priorities.
Additionally, organizations are encouraged to create customized Key Performance Indicators (KPIs) with input from appropriate stakeholders and physician practice leaders.
Citizenship bolsters a progressive, patient-centric, cohesive brand
The last component encompasses factors that drive patient and brand loyalty and growth in a consumer-driven market.
- Patient Satisfaction & Correlating Metrics Press Ganey, an independent organization that conducts patient satisfaction surveys remains one of the top authorities on this metric. CMS uses the Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS). Our model proposes awarding points according to the ratings organizations receive on these surveys—as well as other satisfaction measures specific to the organization.
- Embracing emerging technology and new processes Models should incentivize physicians to explore and embrace novel technologies that advance patient care and increase efficiency. As an example, virtual health services will play a growing role in the post-pandemic world as a powerful solution to manage physical space, resource, and staffing constraints as well as growing provider and patient preference for care outside or away from traditional settings. Metrics can be developed related to telemedicine training, coaching, and utilization. This element may also include rewarding both the use of and continued education and skill development relating to robotics, AI, and the use of advanced technologies, including in support of digital health services.
- Organization Policy & Procedure Compliance Core incentives can include compliance with organizational and clinical policies and procedures, such as appropriate clinical documentation to support billing charges, closing encounters in the electronic medical record to initiate the billing cycle, and attendance at multi-disciplinary case conferences. By factoring these activities into the compensation metrics, both physician and employer benefit.
- Administrative Roles & Promotion of the Organization’s Brand The CBI Model includes compensation for leadership. Leadership activities may include speaking engagements, research publications, service on administrative boards, media/public appearances, medical directorships, medical staff executive committee participation, or service on quality improvement panels or medical supply formulary boards.
An objective, clearly defined methodology builds trust between physicians and organizations
At the core of CBI Model’s success is a framework that requires measurable activities that are routinely socialized transparently to participating physicians. Transparency of the process instills a sense of fairness as well as healthy competition among peers. Physicians who have met the threshold are grouped in performance quartiles in each Core Incentive. It is recommended that the payout for each quartile is weighted to recognize the achievements of top performers. As more physicians qualify for payouts from a Core Incentive, a disproportionately greater percentage of that Core Incentive Funding is released. This incentivizes physicians to encourage participation among their peers to maximize the available incentive funds.
Visualizing the model in practice
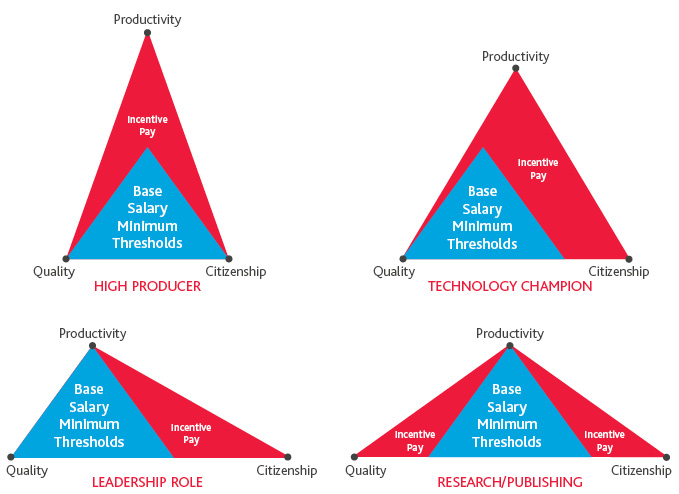
The CBI Model allows physicians to develop and control their personal career journeys, focusing and balancing efforts in productivity, quality outcomes, and citizenship—creating different archetypes for each chosen path.
Prototype
The point-based system allows for individual physicians to have varying career path development. Examples include a physician who chooses to be a high output producer or a physician who chooses to be an early adopter and champion of technology.
Archetypes
Additionally, within each Core Incentive, physicians can occupy different archetypes beyond the traditional focus on pure productivity. For example, three physicians can focus their efforts equally on citizenship points; however, one may have more tenure at the practice and choose to participate in an administrative leadership role as a director of his or her department, while a second decides to focus on researching and publishing scholarly articles that also produce improved clinical pathways for the group, and a third may be more of an early adopter embraces telehealth fully.
Navigating uncertain times: The CBI Model aligns with current and future regulatory trends
While the CBI Model can work in isolation and is envisioned as a stand-alone, new-era physician compensation model, it can work in tandem with value-based payment arrangements and other physician-alignment models, such as CINs, ACOs, co-management and gainsharing. In addition, certain pre-pandemic proposed changes to the “Safe Harbors” under the Federal Anti-Kickback Statute (“AKS”) and to the Federal Stark physician self-referral regulations would, if they become law, support expansion of value-based arrangements and offer new flexibility for physician compensation models designed for the value- and outcomes-based environment.
The CBI model advances the goals of Clinically Integrated Networks (“CIN”) and Accountable Care Organizations (“ACO”)
CINs and ACOs have historically been built around specific sets of measures for Value-Based Care (“VBC”). The measures often include some kind of economic lever to incorporate productivity into the discussion. Definitions for each of these VBC categories may significantly change as a result of the pandemic:
- Quality: Post-pandemic we will need to consider how to measure quality, for example in telehealth, as well as in partnership with health plans, pharmacies and other post-acute care providers.
- Service: Traditional measures of providers (Access) and hours open (Availability) will give way to more relevant indicators of services, such as numbers of telehealth visits, levels of telehealth visits, and time spent for new patient appointments.
- Cost: Cost management and measurement will be focused on technology uses and associated costs and efficiencies.
- Productivity & Other Economic Levers: Revenue generation and cost reduction metrics can pivot to address COVID-19 matters and focus on at‑risk populations.
The Triple Aim commitment of CINs and ACOs to improve the patient care experience, improve the health of populations and reduce the cost of healthcare must be translated into operations and care delivery. Each physician member of a CIN or ACO must actively commit to the Triple Aim and be focused on the data-driven and transparent coordination of care among health systems and other providers. Tailoring incentive compensation is a key tool to drive CIN and ACO success, which can be thoughtfully accomplished through the CBI Model.
These sets of measures have classically been defined by governmental payors with the commercial payor industry following suit and often adding their own nuances. CINs and ACOs represent a unique challenge in that, even in “normal times” one must think and act like both a payor and a provider. The challenge and the to do so post-pandemic will be all the more obvious and challenging. Like all VBC and P4P models before it, the most legitimate and most effective ones will be borne out of collaborative, thoughtful, patient-centered discussions among healthcare providers and healthcare payors.
Co-Management and Gainsharing work alongside the CBI Model to put physicians in the driver’s seat
The CBI Model can be layered with predecessor co-management and gainsharing arrangements or can be designed to work with new complementary programs. Recall that co-management arrangements are oriented and limited to a particular hospital service line, usually orthopedics or cardiac services. Parties typically establish quality measures that are identified, verifiable and evidence-based, and reasonably related to the hospital’s services and patient base for the relevant service line. Compensation includes fixed payments to the participating physicians (or their group) based on administrative contributions, and variable payments tied to achieving established quality targets. Gainsharing arrangements historically have been based on cost savings that are attributable to physician efforts to control the cost of providing care to hospital patients within a particular service line (often cardiology). Gainsharing arrangements are developed around standardization and substitution of products and reasonable use, with safeguards for patient care. Programs are relatively short-term (1 – 3 years) and the metrics are rebased annually. Program “gains” (cost savings) are shared with the participating physicians.
Keeping an eye on future regulation
As a part of the continuing “Regulatory Sprint to Coordinated Care,” which is intended to improve providers’ alignment on an end-to-end treatment approach (that is, coordination among providers along the patient’s full care journey) and to support provider’s efforts to coordinate and collaborate, in October 2019 OIG proposed changes to the AKS Safe Harbors, and CMS proposed changes to the Stark regulations. These proposed changes have not—and may not ever—become law. They nonetheless are further evidence of the dramatic change from a volume-based reimbursement methodology to an outcome and value-based methodology. Under an outcome-driven system, providers need to collaborate to deliver better value.
The proposed AKS rule centers on “value-based enterprises.” A value-based enterprise consists of two or more participants entering a written agreement to improve the coordination or management of patient care, improve quality of care for a certain patient population, or reduce costs to payors while maintaining quality. Value-based enterprises would not include: (1) pharmaceutical manufactures; (2) manufacturers, suppliers, and distributors of durable medical equipment, prosthetics, orthotics, or supplies; and (3) laboratories. The proposed rule includes new Safe Harbors for care coordination arrangements, financial risk arrangements, patient engagement activities, and donation of cybersecurity technology and services. The proposed rule modifies the personal services and management contracts Safe Harbor to add support for outcomes-based compensation.
The proposed changes to the Stark regulations would add an exception for value-based arrangements (with characteristics similar to value-based enterprises as proposed under the AKS Safe Harbors) as well as exceptions for certain financial risk arrangements. The proposed Stark changes also clarify that, for employed physicians, a productivity bonus does not take into account the volume or value of the physician’s referrals solely because corresponding hospital services (inpatient or outpatient hospital services, which are Stark designated health services) are billed each time the employed physician personally performs a service. In the preamble to the proposed rules, CMS reaffirmed that its intent in interpreting and implementing the Stark law has always been ‘‘to interpret the [referral and billing] prohibitions narrowly and the exceptions broadly, to the extent consistent with statutory language and intent,’’ and, it says, “we have not vacillated from this position (66 FR 860).”
A model suited to address our post‑pandemic world
These alignment models and proposed updates to the AKS and Stark laws support and reinforce the timeliness of the CBI Model and harmonize with its underlying principles. The COVID-19 pandemic has hastened and sharpened the health industry’s focus on the need for such coordinated, cradle-to-grave care that emphasizes the use of advanced technology to offer the right care, at the right time, and in the right setting, all of which the CBI Model promotes.
Key Takeaways
1. Unpredictable environmental circumstances like the COVID-19 pandemic create an environment where physicians seek financial stability but are reticent to surrender their autonomy. Hospitals are similarly constrained and look to prioritize shared risk/reward relationships. This yields an opportunity to revisit compensation models and explore compromises most likely to lead to mutual resilience in uncertain times.2. Establishing a new compensation model may be challenging; however, by implementing a new model now, both large and small organizations can encourage loyalty from their physician partners and enjoy more flexibility in the development of their programs.
3. Ultimately, successful compensation models of the future, such as this CBI Model, require customizable levers to incentivize providers based on their tenure, quality outcomes, allegiance to mission, and degree of clinical and extracurricular engagement, as well as the strategic needs of the organization.
The views and opinions set forth herein are the personal views or opinions of the authors; they do not necessarily reflect views or opinions of the law firm or advisory firm with which they are associated.
SHARE