A Checklist for Managing Patient Surge During COVID-19
Upstream & Downstream Care Coordination, Workforce Respite & Virtual Health are Critical
As the novel coronavirus (COVID-19) pandemic continues to spread within the United States, hospitals’ top priority is providing patient care and limiting loss of life. To effectively do that, they must be able to safely and ethically address the drastic surge in patients they’re already seeing.
During the pandemic’s peak in Wuhan, about 25 per 10,000 adult COVID-19 patients were hospitalized, with about 12 per 10,000 adults considered to be in serious condition and nearly 3 in 10,000 adults needing critical care each day. The U.S., meanwhile, has about 5,200 community hospitals and about 924,000 staffed beds across the country, according to the American Hospital Association (AHA). About 97,000 of those beds (or just 10%) are classified as intensive care beds. To put it into perspective, the U.S. has 2.8 hospital beds per 1,000 residents while China has 4.3 per 1,000 residents and Italy 3.2, according to the Organization for Economic Co-operation and Development.
Here are the questions—and related actions—hospital leaders should consider when addressing the surge in patient care demand:
1. Have we created a crisis command center and designated clear swim lanes for who is managing the crisis and ensuring business continuity?
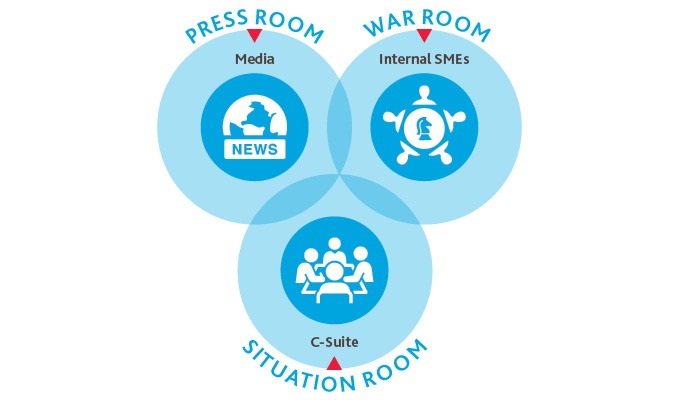
Designate a situation room, which should include your organization’s most senior leaders. They should map out the most important questions the organization needs to consider for the short term and long term, make important decisions around each based on intel shared by the war room, and communicate those up to the C-suite or board of directors. Examples of the types of questions they should consider include:
-
How many of our partners on the care continuum, labs or other vendors are in locations with higher outbreaks of COVID-19? Can we help them address capacity issues?
-
How many beds or critical care areas do we have at our disposal in each of our facilities? When are we likely to have a bed shortage, and what plans should we put in place—and who should we engage outside our organization—to address that?
-
What are our community’s most significant concerns, and how do we address those publicly?
-
What equipment do we have at our disposal to provide telehealth to certain patient populations, and how do we need to train our clinicians and support staff to successfully do that?
-
What facilities can we transform on or off-site to provide our frontline clinicians respite during this crisis?
-
What are the statistics for incidence of transmission so we can track the progress of covid-19?
-
Have we instituted emergency credentialing procedures to maximize our healthcare workforce?
-
Have we instituted a “call tree” for senior members of the hospital?
Designate a war room, which should consist of a diverse group of leaders across the organization (human resources, IT, supply chain management, finance, communications, etc.) who are responsible for finding the answers to key questions and relaying that intel back to the situation room to inform their critical organizational decisions.
Designate a press room, which consists of senior communications and public relations specialists to manage the ongoing communications of the decisions made by the situation room to both internal and external stakeholders. This team must determine how, when, to whom and at what cadence communications are shared. They are also responsible for maintaining brand reputation both internally and externally.
Establish a daily crisis command center huddle with reports from all three critical areas so you share daily updates at the beginning of each day, identify new questions or challenges, and stay aligned on progress moving forward.
2. How can we transform our existing infrastructure to suit a crisis environment and engage with community organizations to help?
Determine which of your unused or underused physical spaces you can reactivate to meet testing, triage areas and isolation rooms. Evaluate which of your units you can safely turn into private rooms with the equipment—and ventilation systems—necessary to treat COVID-19 patients.
Create a scenario map for managing different types of patients, including separating the worried well patients from your worried symptomatic ones. Designate certain areas outside the hospital to intercept worried well patients, answer their questions and provide them guidance on where to go instead of the hospital if their care needs are not urgent and they have no existing health conditions. Clearly outline when and where they should seek testing and/or emergency health services. For patient populations known to be at greater risk of the virus—including those with compromised immune systems, chronic diseases, the elderly and others—designate other, quarantined areas for their treatment.
Confirm how many elective or non-urgent procedures you have scheduled, and which can be postponed. To protect patient safety and free up more rooms and hospital beds, evaluate which scheduled procedures can be safely postponed. Consult guidance from the Centers for Disease Control and Prevention (CDC), the Centers for Medicare & Medicaid Services (CMS) and the American Hospital Association (AHA) to determine how to approach these decisions.
Engage the public sector—as well as other private sector entities across industries—about using empty facilities in your community to meet rising patient demand. Once confirming capacity and patient care approach with your partners on the care continuum, you should have an idea on the number of facilities and beds you need to meet patient needs. Repurposing community centers or other currently empty facilities to provide those facilities is an option worth pursuing, but it requires proactive collaboration between the public and private sectors.
3. Can we streamline processes for patient transfers between sites, support capacity demand, and share information, staff or supplies?
Reach out to primary care providers in your patient care area to intercept their patients before they arrive at the hospital. Get a sense of how many patients they’re treating or counseling with suspected COVID-19 symptoms, and make sure they’re advising patients when and under what conditions they should visit a hospital and when they should recover at home. Confirm they know where alternative testing sites are and that they’re communicating that information to patients to help mitigate an overload of non-urgent patients into the emergency department.
Reach out to downstream post-acute care providers in your area. Since the elderly and people with existing health conditions are most impacted by the virus, many who will need critical care support will have to be discharged to a post-acute care setting after the hospital to recover. Confirm with your post-acute care partners their existing capacity and plans to mitigate capacity challenges, including ways to expedite the discharge process and potentially have patients finish recovery in their homes. Aim to give them a 48-hour notice period for when you’ll be transitioning patients from your facilities to theirs for further recovery.
Identify the retail clinics or other outpatient resources in your community and confirm which ones are offering certain services like on-site or drive-through testing. Identify the process people should follow to receive such services, and coordinate communications to various patient populations as appropriate, sharing information about their diagnostic and treatment services and products with appropriate patient populations. For example, for your worried well patient group, you could proactively share with them the various retail clinic resources in their area that may be offering virtual wellness checkups, on-site or at-home diagnostic services, or other health and wellness products that could be delivered to their homes should they have concerns about symptoms.
Coordinate supply inventory for high-demand personal protective equipment (PPE), monitoring availability through current suppliers as well as outreach to nontraditional suppliers. Alternative sources could include outreach with requested needs to regional and/or community health resources, industry leaders on your governance boards as well as allied industries for PPE such as construction.
4. What impact could this crisis have on our workforce, and how can we address that?
Maintain transparent communications with your workforce, particularly frontline clinicians, and acknowledge the increased risk they’re taking on. Address PPE shortages and near- and long-term plans to address them, creating policies and procedures around making sure existing PPE supplies go as far as they can in a way that preserves patient and clinician safety.
Establish a regular cadence of communication and determine what types of information are best suited to certain types of channels. For example, sensitive information will need to be communicated through a channel different from updates on the daily movements of staff and changes in personnel policies. Other types of updates—particularly urgent ones that staff across the organization must be made immediately aware—may need to be communicated through push notifications.
Take action to preserve the health and safety of your staff and mitigate stress and anxiety. Weigh the possibility of certain clinicians and/or non-patient-facing staff only working evenings and others only working days, to give both groups a chance to rest while also diversifying potential risk to your overall workforce. Ensure that when you’re considering swing or switch schedules, you acknowledge their financial implications. For example, some staff may not want to miss out on shifts because that means they’re not bringing in as much income to their families, while others may have greater financial flexibility. Engage your workforce and gather their personal input when making these decisions and give them a say.
Consider which of your departments can realistically work remotely. Finance, IT and human resources, for example, are likely easy switches to remote. Evaluate whether you can repurpose their physical office space to suit other more urgent patient and/or workforce respite needs during this time.
Provide on-campus respite for your staff. This includes food and other supply delivery services and areas for staff to rest, meditate, shower, worship or exercise. This could also include offering on-site therapy or support groups and providing on-site catered meals since clinicians may be unable to get groceries or go home for long periods.
Establish procedures for increased cleaning of campus surfaces and emphasize the importance of hand washing and other basic sterilization processes.
Engage local nursing and medical school students and train them on how to manage upstream and downstream communications to patients and their families. While students may not yet be qualified to provide the actual patient care, they are comfortable in a healthcare environment and can add lift to frontline clinicians by taking communications off their plate and helping to manage patient flow and care coordination.
Engage retired nurses or physicians to mitigate the aggravated clinician shortage during this time. Provide training specific to your hospital so they can quickly provide added patient care support. Implement emergency credentialing procedures mandated by the Joint Commission on Accreditation of Healthcare Organizations to satisfy clinical needs.
5. How can we leverage telehealth to screen symptoms with a doctor before a patient comes to the hospital, limit exposure that could infect patients and clinicians, and free up hospital capacity?
Engage and activate your patient base to telehealth. Telehealth has arrived and all stakeholders are embracing it. During the pandemic, providing telehealth services is a civic defense strategy at heart, but soon it will become the standard of care and evolve into larger opportunities. Your patient base will quickly want to use telehealth in its care, especially during the pandemic. Now is a good time to be proactive in educating and engaging your patient populations. When in-person visits are on hold, telehealth visits can both take care of your patients’ needs and provide a source of revenue generation. Telehealth and virtual health overall represent the future, and the future is here.
Review temporary telehealth guidelines considering COVID-19. Effective March 6, CMS is temporarily allowing Medicare and Medicare Advantage to reimburse clinicians for telehealth services provided to beneficiaries across the country in all care settings at the same rate as in-person visits. Health Care Service Corporation/BlueCross BlueShield also announced coverage for telehealth visits, with all major insurers closely following suit.
Determine what equipment you have at your disposal to provide telehealth services on an emergent short-term basis. CMS’s waiver also authorizes the use of phones with audio and video capabilities for the furnishing of Medicare telehealth services, removing previous confusion over what technology is approved for such services. Health and Human Services (HHS)’s Office for Civil Rights (OCR), meanwhile, will exercise enforcement discretion and waive penalties for noncompliance with HIPAA Rules against providers that serve patients in good faith through communication technologies listed in the Notification of Enforcement Discretion for Telehealth. For some appointments, a simple check-in over the phone without video may suffice.
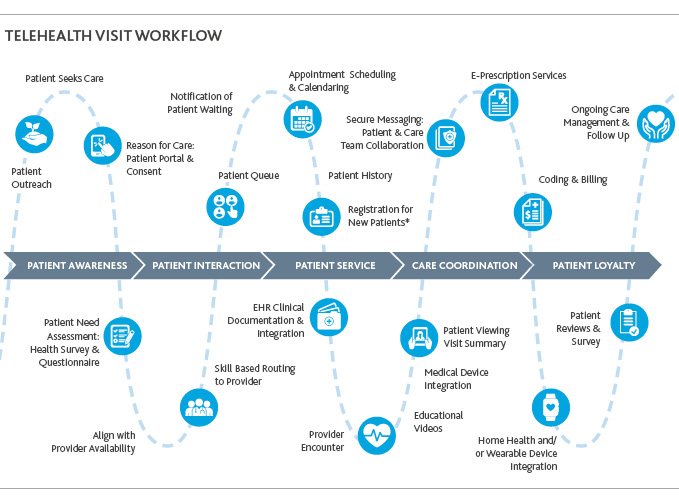
Develop a long-term integrated virtual health plan that maps out what a telehealth visit workflow looks like at your organization for the future. The future virtual visit may require more sophisticated equipment with a higher level of personalized experience (i.e., sharper images, professional backgrounds, reliable connections and other features). A successful virtual health visit will support patient awareness, patient engagement, patient service, care coordination and ultimately, patient loyalty. User experience and potential pain points should be key components of your plan, and you should determine appropriate change interventions and patient engagement activities. Clinician training should also be incorporated into your plans, and addressing various comfort levels with technology across provider generations will be a key component of this.
Identify low-hanging fruit for rapid activation of telehealth. While it is important to consider the end-to-end telehealth workflow for strategic direction, you can also implement a few aspects of the process rapidly to meet the immediate needs. Many organizations have already deployed some form of video-conferencing solution that can meet the tactical needs of the pandemic. Beyond video conferencing, organizations should consider deploying a portal and a bot to take the brunt of the patient influx. A patient portal can be used to provide information about the pandemic, overview of the telehealth process, as well as consent that can be logged if the patient agrees to move forward with the telehealth visit with a care provider. A healthcare-focused bot can help patients self-assess their condition based on clearly identified criteria of the virus and to answer frequently asked questions before an actual clinician needs to be engaged.
Consider performance and cybersecurity requirements of the telehealth solution. A tactical deployment of a video conference solution may meet the immediate needs. In many cases, however, such solutions may not be adequate to meet the performance requirements of the patient influx, which will have direct impact to user experience. It is also important to make sure that you address the cybersecurity requirements of your organization as new technology solutions are introduced to the environment.
Review the patient cost-share waiver. Medicare’s coinsurance and deductible would generally apply to these telehealth services. However, HHS is providing flexibility to healthcare providers to reduce or waive the cost-sharing of such services reimbursed by federal healthcare programs. If the 1135 waiver requires an established patient relationship, HHS has said it will not conduct audits to ensure that such a prior relationship existed for claims submitted during the pandemic.
SHARE