Stark Overhaul Could Boost Value‑Based Care, Increase Tech’s Healthcare Opportunity
Read our most recent insight Five Tips for Renegotiating Your Value-Based Care Contracts to help prepare when renegotiating your organization’s contracts.
Changes Would Require Providers to Have Clear Data Ethics Framework
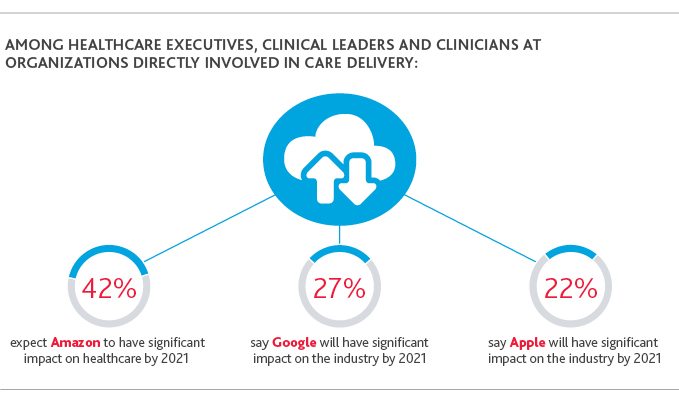
Healthcare organizations have already turned to tech giants like Amazon, Microsoft, Google and Apple for their cloud storage services to more effectively store and analyze health and other data, with the goal of improved care outcomes and product innovation. Doing so is critical to their survival in an industry increasingly being reimbursed based on quality of outcomes rather than quantity of services.
For hospitals—whose traditional revenue streams are coming under fire from all directions—analyzing patient data correctly for the purposes of research and development and improved care outcomes can be a lifeline. Big tech companies, sensing the opportunity data storage represents in healthcare, are already fighting for dominance in the industry.
Recently proposed updates to the Anti-Kickback Statute and Stark Law, from the Office of Inspector General (OIG) and Centers for Medicare & Medicaid (CMS), respectively, would make analytics an even more important lifeline for providers—and in the process, expand tech’s influence in healthcare. This would require provider organizations to shift from thinking about how patient data can be used to how it should be used.
*Source: BDO/NEJM Catalyst buzz survey
Tech’s Opportunity
We expect the proposed overhauls of healthcare’s anti-corruption laws to unleash a wave of value-based contracts in healthcare. This will open a new window for tech companies in the areas of documentation and analytics.
Under value-based contracts, organizations are financially rewarded or penalized not only for their own patient outcomes, but also those of their partners in care delivery. To succeed in such an environment, it becomes critical for organizations to partner with, and refer patients to, organizations with strong outcomes, and to be able to track and analyze those outcomes.
However, in their current forms, Stark Law and the Anti-Kickback Statute, prohibit:
- The referral by a physician of a Medicare or Medicaid patient to an organization if that physician has a financial relationship with that organization
- The exchange of anything of value to influence the referral of business reimbursable by federal health programs
OIG’s and CMS’ proposed overhauls, released on Oct. 9, are aimed at encouraging more providers to transition from fee-for-service care models to value-based ones by relaxing certain compliance barriers to doing so. The overhauls would add new safe harbor protections under the Anti-Kickback Statute and create new, permanent exceptions to Stark Law for value-based arrangements made in the interest of better care coordination and improved patient outcomes.
For example, CMS’ proposed exceptions for compensation arrangements under Stark Law include one that would apply to a value-based arrangement where a participating entity has, during the entire period of the contract, “assumed full financial risk from a payer for patient care services for a target patient population.”
Being able to accurately document and analyze sometimes disparate financial risk under such arrangements—and show how those arrangements are indeed benefiting target patient populations through improved outcomes—will be key for providers to manage risk. More broadly, the quality of the data that providers collect under value-based contracts, and how they evolve their care models according to the stories the data tells, will dictate the success of value-based care.
Balancing Data Analytics with Data Ethics
At the same time, as the use of data analytics and documentation becomes even more important to healthcare providers, they—along with their partners and tech vendors on the continuum—must make data ethics an important part of the conversation.
Shifting from a focus on how personal data can be used to better improve patient outcomes to how it should be used is key.
Providers can start that conversation by establishing a data ethics framework. Key considerations include:
- Clearly defining value-based arrangements and their benefits: Be clear about what you’re trying to achieve through the arrangement, what issues you’re trying to solve and for which patient populations you’re trying to solve them.
- Develop a transparent program that holds your organization and partners accountable for the use of your patient and health data: Be transparent about the use of personal data and take accountability to protect it. This includes giving your patients knowledge of the data you’re collecting and how it will be used.
- Use data proportionate to your value-based arrangements: Only use the minimum amount of relevant data necessary to achieve and demonstrate the arrangement’s specific results. Before starting the arrangement, determine the types of data you and your partner need, the source of it and how you will receive it.
- Understand data limitations: This means understanding the source of your and your partner’s data, including metadata, what processes are in place to maintain the integrity of your data, and whether caveats will be necessary to future policies or procedures.
Providers with the most accurate documentation and data analytics—executed under clear data ethics frameworks—will thrive under the future value-based care state and be best positioned to manage compliance risk.
SHARE