Closing the Gap: Addressing Healthcare Disparities in Black Communities
Addressing the root causes and impact of healthcare disparities is essential to creating health equity, which is needed for a more fair and just society. The COVID-19 pandemic has shed light on the issue of equitable access and quality of care. But the history of these issues in the healthcare industry extends well beyond the last two years.
Despite their long history, health disparities can be addressed with actionable steps by hospitals, hospital leadership and neighboring communities. Understanding the impact that slavery and segregation in the United States has had on the provision of medical care to Black-American communities can help leaders understand how we got to where we are today. It can also help set the course for what’s needed to eliminate biases and create a new standard of health equity. Specific strategies and initiatives to ameliorate the past misgivings are needed, not just for talk, but to create real change.
History of Healthcare Disparities and Black Americans’ Contributions to Medicine
Healthcare disparities are more than simply a difference in the delivery of healthcare to different populations. They are differences that persist after patient choice and clinical variables are adjusted for. Examples include noticeable differences in the following:
-
Disease morbidity and mortality
-
Patient-reported outcomes to diseases
-
Access to healthcare providers, novel medicines and
-
advanced technology
The origin of these disparities can be traced back to the onset of American slavery in 1619 during which there was little concern for the health of enslaved people. Today, healthcare disparities persist because of both a pattern of implicit bias and a history of overt discriminatory behavior toward racialized and marginalized communities trying to access the healthcare delivery system in the U.S.
Ironically, slaves did not receive proper healthcare despite the fact that they were viewed as valuable commodities by their owners as evidenced by the common practice of insuring the owners against their loss. Slaves lived under difficult conditions with poor nutrition and little access to medical treatment. Healthcare disparities intensified as slavery continued into the 19th century. However, in 1865, the 13th Amendment outlawed slavery, stating, “neither slavery nor involuntary servitude, except as a punishment for crime whereof the party shall have been duly convicted, shall exist within the United States, or any place subject to their jurisdiction.” But despite the illegality, a two-tiered system of healthcare emerged in the U.S. where Black Americans had different access and treatment than their white American counterparts.
Because of persistent healthcare inequities, the Black population took steps to improve its own healthcare by training doctors and developing medical facilities owned and operated by their community. The first Black hospital and medical school were established in 1868 at Howard University in Washington, D.C. Between the years 1865 and 1904, fourteen Black medical schools were created.
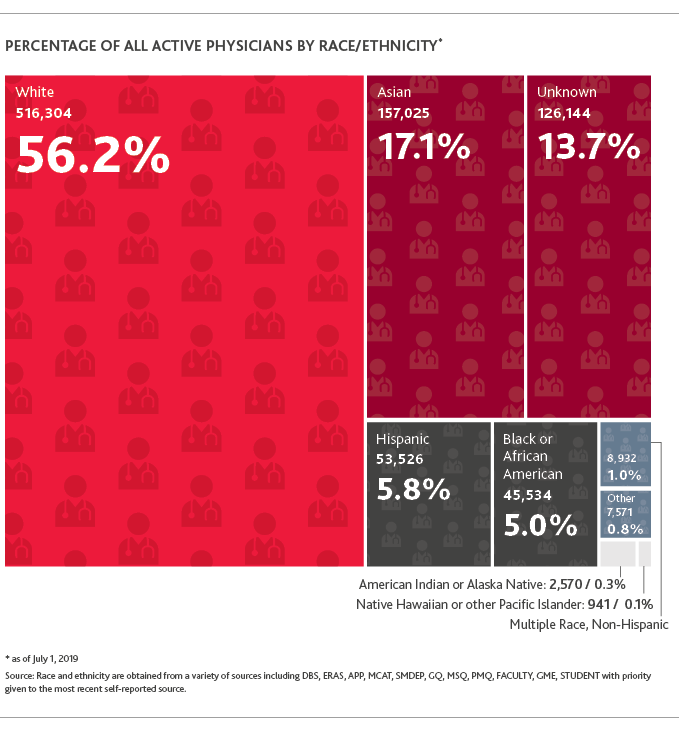
In 2021, there was a 21% increase in the number of Black or African American medical students accepted into the first-year class, but that still totaled just 2,562 students. The Association of American Medical Colleges notes that as of 2019, Black Americans represented 5% of the total population of physicians in America, and there are several references highlighting the barriers to some of the coveted subspecialties.
What Are the Social Determinants of Health?
There are five factors that make up the social determinants of health:
-
Economic status
-
Educational attainment
-
Environment
-
Access to healthcare
-
Community and social support
Impact of Racism on Black Medical Care
On patients
The issue of racial and ethnic disparities in healthcare will not be overcome until we also focus on the impact of the social determinants of health (SDoH). Strong ties between healthcare disparities and the SDoH are far from coincidental. Given the long history of racial and ethnic segregation in the U.S., the links between healthcare disparities and SDoH explain why a person’s zip code is more likely a greater determinant of their health outcomes than their genetic code. It’s important to evaluate a patient’s lived experience and recognize that many of the factors contributing to a difference in healthcare outcomes are neither ethnically or biologically based but are instead a function of the structural environment in which the patient lives.
Multiple biases and misconceptions about race continue to affect the delivery of medical care. For example, many Black patients are perceived to have a higher pain tolerance than other races, so they’re more frequently denied pain medication. Also, patients with skin disorders and other dermatological issues are often treated differently based on skin color, despite no scientific evidence supporting the need to do so. There is no evidence behind the myth that the skin of a person of color is thicker than a white person’s skin, so X-rays and other radiation modalities do not need to be conducted differently. And despite other perceived physical differences, there is no biological proof that defines humans as one race versus another. These facts underscore the reality that race is a social construct, not a biological one.
On doctors, clinicians, and nurses
The practice of racial concordance, where a physician and a patient have a shared racial identity, is seen as one way to overcome healthcare disparities. But the ratio of the Black population to the availability of Black doctors, especially in underserved communities, presents challenges. Right now, just 5% of the total physician population in the U.S. is Black, despite the fact that Black Americans comprise over 13% of the U.S. population.
The cause of this disparity lies in structural barriers and inequity. The number of Black medical students who have to take out loans for their education is significantly greater than their white counterparts. Physicians of color also report being discouraged from pursuing sub-specialty practices, often leading to overall lower earning potential.
There is also a credentialing process that physicians must go through in order to get hospital privileges. Biases in this process are barriers for some providers. Then, once a physician is settled in practice, the cost of living tends to be greater for physicians of color who may face higher interest rates on loans for home, cars or practice capital expenses. Healthcare disparities will not be resolved until the underlying racism within the policies and procedures of health institutions and the business community is recognized and addressed.
Taking the Next Step Forward
In order to achieve equity in the healthcare industry, it’s necessary to create a collaborative effort that includes policymakers, hospital systems, healthcare administrators, practitioners, medical schools and patient advocacy groups. Focusing on ending discrimination is not enough to address all the present-day healthcare disparities. The goal should be to move beyond the absence of discrimination, beyond the presence of equality and onto a stage of equity and justice, so that we can improve overall health and quality of life for all Americans.
Hospital leadership’s role
One approach that attempts to make progress toward this goal is having physicians and other clinicians take courses in cultural competence. This includes learning about and undoing their own unconscious bias and, in some cases, having their conscious bias amended. BDO’s 2021 Health Equity Survey found that nearly half of hospital executives (49%) say their top objective for training employees on health equity and healthcare disparities is outlining how unconscious bias can influence attitudes, behaviors and expectations related to health, medications, treatment regimens, healthcare and healthcare providers.
Within hospital walls, it’s important for Black doctors to nurture and mentor current medical students and show them the history of what people have overcome and what they can do. By establishing a safe, inclusive and tolerant hospital environment, those in leadership positions can achieve better outcomes for all. According to the same survey, 37% of healthcare organizations already have a health equity strategy, and another 37% are planning to implement one in 2022.
From a corporate perspective, large hospital organizations and associations can lead the way toward a more equitable healthcare system. For example, the American Medical Association (AMA), founded in 1846, has recently taken action by making a declaration that health inequity has no place in American medicine and committing to eliminate health inequity with actionable steps. They appointed a diversity, equity and inclusion (DEI) director and have set an agenda with timestamped goals to ensure these barriers to health equity are removed. As an organization that had previously excluded the Black community from its membership, these are welcome actions by the AMA.
Other organizations are also making progress. The Association of American Medical Colleges (AAMC), a group that oversees 140 medical schools, now provides guidance for opening opportunities to minority students. The American Heart Association (AHA) reviewed its own legacy of discrimination and racism, and it has published a presidential advisory on the role of structural racism in healthcare disparities and initiated a DEI editorial panel. Just like in the corporate world, where people with diverse backgrounds need to be in boardrooms and committee rooms, in the medical world, people of color need to be in leadership and decision-making roles, such as on the editorial boards of medical journals.
Individual and community roles
COVID-19 has shed a spotlight on the challenges that impede the delivery of equitable healthcare in the U.S. The pandemic has made people recognize disparities regarding healthcare delivery, especially with the disproportionate impact of mortality and morbidity in communities of color, which are more severely affected by the disease.
The pandemic also highlighted the ongoing need to be open to other people’s views, including reading and consuming media with viewpoints different from one’s own. Change is uncomfortable, but the sooner we put in the work, the sooner we can eliminate future discomfort and improve equity, especially for marginalized communities.
Everyone can engage in supporting improvements in public health education and growing health equity. Misinformation has done damage to communities of color, especially with regard to healthcare. With individual advocates, allies beyond communities of color and the support of every aspect of society and government, we can work toward remediating the problem of racial and ethnic disparities in the medical community and set ourselves on track for a more equitable future.
Further Reading:
-
Blacks in Medicine: Clinical, Demographic, and Socioeconomic Correlations by Dr. Richard Allen Williams.
-
Healthcare Disparities at the Crossroads with Healthcare Reform edited by Dr. Richard Allen Williams.
-
Why Your ZIP Code Matters More Than Your Genetic Code: Promoting Healthy Outcomes from Mother to Child by Garth N Graham.
-
An American Health Dilemma, by W. Michael Byrd and Linda A Clayton.
Insights based on a BDO-hosted webinar held by Dr. Walter Clair (Vice Chair for Diversity and Inclusion, Vanderbilt Department of Medicine) and Dr. Richard Allen Williams (Founder of the Association of Black Cardiologists, and Founder of the Minority Health Institute), entitled “Healthcare Disparities Within Black American Communities: How We Got Here and How to Close the Cultural Gap.” To access the recorded session, moderated by BDO’s Dr. Herman Williams and Tiffany Prudhomme, click here.
SHARE