Unleashing Nurse-Led Innovation
Table of Contents
- Executive Summary
- U.S. Health System Looks to Nurses for Innovation—Just Not at the Leadership Level
- Today’s Changes Will Unleash More Nurse Innovators by 2025
- Nurses are Addressing Today’s Top Health Challenges
- The Role of Design Thinking in Producing Greater ROI
- Nursing a System-Wide Change in Mindset
Executive Summary
When Diane Spatz first began working to more effectively promote breastfeeding vulnerable infants, it’s unlikely she thought of it as an act of innovation.
Yet innovating is exactly what she was doing when she turned her own extensive clinical experience as a nurse into a 10-step solution for improving the care of our most vulnerable infants starting life in the neonatal intensive care unit (NICU). The process developed by Spatz, PhD, RN-BC, FAAN, Professor of Perinatal Nursing and Helen M. Shearer Term Professor of Nutrition at the University of Pennsylvania School of Nursing and Director of the Lactation Program at Children’s Hospital of Philadelphia, has now been implemented in hospitals around the country and the world.
And it’s proved successful. Before implementation, the percentage of NICU infants at Children’s Hospital of Philadelphia receiving human milk at discharge was about 30 percent. In 2014, six years after it was implemented, more than 86 percent of NICU infants were discharged on human milk.
Spatz, and other nurses like her, are proof that nursing innovation—unleashed through human-centered design, expanded scope of practice, advanced education and executive leadership—is already happening.
We also know this to be true through our team of clinical and business innovation leaders who have seen nursing innovation gain speed over the course of their careers. We’ve worked with clinicians practicing at advanced levels and advising companies on product development, leaders of global research initiatives around social determinants of health and advisers to some of the top health systems in the country. And nurse innovators have been by our side all along the way.
But nursing innovation has yet to be fully unleashed.
That’s why, together with Penn Nursing, BDO embarked on a mission to find out how it’s being unleashed today—and what health systems and communities need to change to create a future where nurse innovators are all practicing at their full scope.
To do this, we surveyed clinical and business leader stakeholders themselves—including at hospitals, post-acute providers, payers, biotech and med device companies—on where they’ll find the most value from nursing by 2025.
What we found is that organizations across the system are already looking to nurses for individual-level innovation and clinical acumen skills. But they’re missing out on the opportunity—including improved patient outcomes—that comes from bringing nurses into innovation at the leadership level.
If true care transformation is to take shape, health systems and businesses must recognize that nursing can and must extend well beyond the bedside and the community—and into the boardroom. Nurses are already leading sweeping innovations at larger, systemic levels within clinical and business organizations. They’re just having to navigate around certain roadblocks to do it.
To create a consumer-centric health system capable of addressing perplexing health issues like the opioid crisis, caring for the aging population and chronic care management, roadblocks need to be removed and systems must embrace nurses as leaders in innovation.
Unleashing nurse innovators is a care imperative and a business imperative.
Read on for Unleashing Nurse-Led Innovation.
U.S. Health System Looks to Nurses for Innovation—Just Not at the Leadership Level
Kathy Bowles noticed a trend: Elderly patients were all too often ending up back in the hospital soon after being discharged.
There was a missing link, and Bowles, PhD, RN, FAAN, set out to find it by posing a question: What was driving these readmissions?
After conducting research into the discharge process and readmission rates of elderly hospital patients, informed by her days as a critical care nurse, she pinpointed a group of high-risk variables that predicts which elderly patients are likely to need post-discharge skilled care: their walking ability, length of hospital stays and presence of a caregiver at home.
Her findings evolved into a decision-support methodology to ensure patients have the post-acute support they need after discharge. The methodology then informed a software product, and later spawned a company, to help hospitals determine the post-acute care needs of their patients and optimize their care coordination.
Bowles is just one example of the many nurse innovators leading the interventions necessary to create transformative processes and products across the care continuum—on both the clinical and business sides of care.
“When people think about nurses, most view them as caregivers. They don’t really think about nurses as innovators or the impact nursing can have when it’s applied to creating research-driven, innovative health solutions—both products and processes,” said Therese S. Richmond, PhD, CRNP, FAAN, Andrea B. Laporte Professor of Nursing and Associate Dean for Research & Innovation at the University of Pennsylvania School of Nursing, where Bowles is preparing the future generation of nurse innovators as Professor and van Ameringen Chair in Nursing Excellence. “Every product and process that touches a patient goes through a nurse. Bowles, and others like her, demonstrate how nurse-led innovations can spearhead care transformation—when they are fully unleashed.”
Yet when it comes to fully unleashing nurses’ potential as innovators, industry stakeholders have some catching up to do.
Though both clinical and business leaders value the innovation and clinical acumen skills nurses bring to their organizations at the individual level, they’re missing an opportunity by not elevating them to the leadership levels needed to fully transform care.
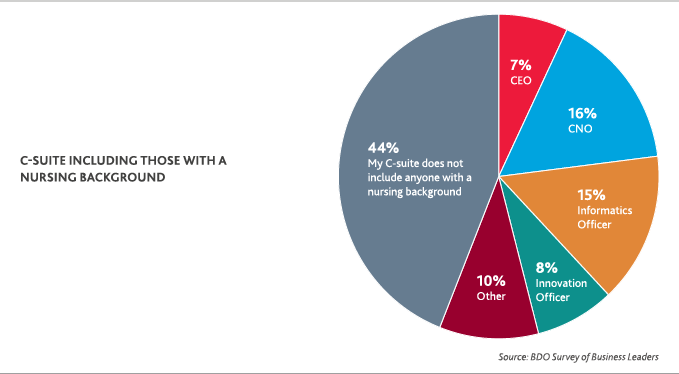
Today, just 31 percent of clinical leaders say they have a designated nursing leader whose primary responsibility is innovation, according to Unleashing Nurse-Led Innovation. Among other industry business leaders meanwhile, just 46 percent say their C-suite includes someone with a nursing background.
Kelly Robke, MBA, MS, RN, Vice President of Thought Leadership at the global medical technology innovator Becton Dickinson (BD) and a nurse for almost 30 years, understands just how important it is to change this.
Robke has spent her career at the intersection of nurse innovation in both clinical and business settings. She views nurses as the leaders of care execution and chief advocates for patients and their families. Because of that, she emphasizes the importance of health organizations elevating nurse innovators to the systemic leadership level if they want to truly transform patient care.
“It’s crucial for the health system—especially business leaders looking to develop patient-centric solutions—to engage nurses early and often,” Robke said. “This doesn’t just mean within the traditional product development process. It also means getting their buy-in on how to commercialize, implement and educate around the solutions, especially if it involves process change or technology.”
Nurses also have an important role in unleashing themselves as innovators and leaders of care transformation: They must claim a seat at the leadership table.
That’s where education comes in, explains Bonnie Clipper, DNP, MBA, MA, RN, VP of Innovation for the American Nurses Association, which educates nurses nationwide through conferences and webinars.
“When we go around the country and talk about innovation, nurses tend not to see themselves in that light, even though they are natural innovators. If I ask a room full of nurses whether they see themselves as innovators, just a couple hands go up. When I reframe the question—to ask if they’ve created a work-around or MacGyvered anything to take care of their patients—all hands go up.”
Changing the thinking around nursing innovation is important: It doesn’t just involve new technologies. It’s taking new ideas created by nurses at all levels, rapidly and rigorously testing them, and putting them into practice across the entire care continuum.
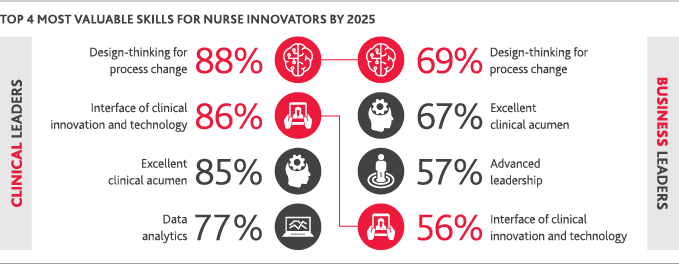
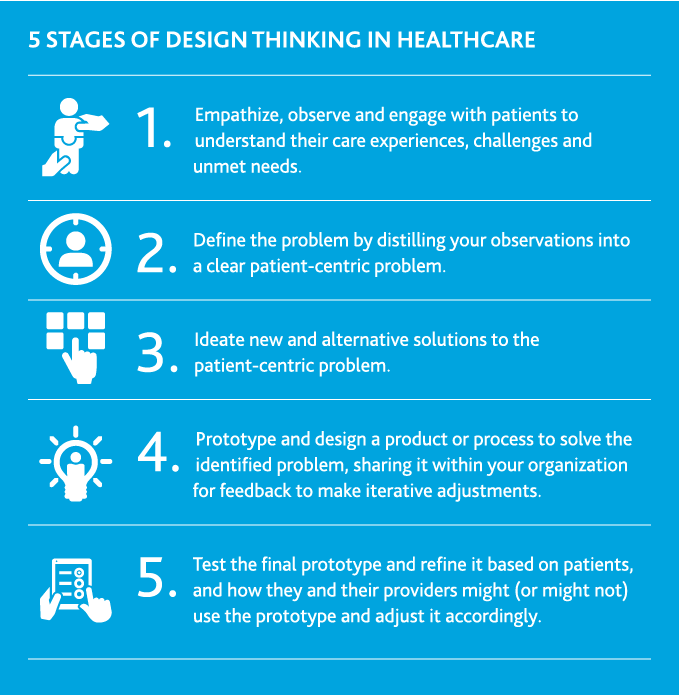
Newly designed educational curriculums focused on innovation skills and design thinking (ranked as valuable skills for nurse innovators by 2025 by both clinical and business leaders), nursing innovation labs and events like hackathons will be key to changing that mindset.
When it comes to defining nursing innovation, it’s perhaps best left…undefined.
Nursing innovation can include developing small, everyday or larger-scale processes, projects and products with the goals of improving holistic care quality and safety; designing and putting into practice new approaches to care delivery; helping all providers improve their care; and communicating health information in an easier-to-understand way for patients and their families—and broader community populations.
We believe, in partnership with others on the care continuum, nurses are best able to solve systemic problems through applied design thinking: looking at issues through the eyes of patients and determining what innovations will work best within each population.
As the front line to care and those communicating most regularly with patients, nurses have perhaps the most realistic—and unlimited—view of patients. Why box that potential in with a specific definition?
 Marion Leary, MPH, MSN, RN, FAHA
Marion Leary, MPH, MSN, RN, FAHADirector of Innovation
Penn Nursing
Today’s Changes Will Unleash More Nurse Innovators by 2025
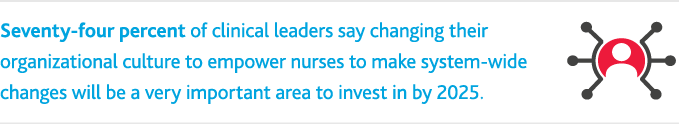
The changes happening today to unleash nurse innovators are likely to shift the leadership makeup at health organizations by 2025.
Organizations on both sides of the industry—clinical and business—signal that avenues to elevate nurses’ individual innovation and clinical skills to the broader, systemic leadership level will be an important part of their path forward.
More than three-fourths (81 percent) of clinical leaders say investing in placing nurses as decision-makers on all strategic planning teams will be very important for health organizations by 2025. Among business leaders, more than half (57 percent) say advanced leadership is a skill they’ll view as very important to nurse innovators within their organization.
By placing emphasis on both bolstering nurses at the strategic decision-making level and leaning on their advanced leadership skills, clinical and business leaders—two of the most important health system stakeholders—are signaling that they’ll look to nurse innovators to help lead care transformation.
To prepare nurses for this elevated leadership role, education will be key, says Antonia M. Villarruel, PhD, RN, FAAN, Margaret Bond Simon Dean of Nursing at the University of Pennsylvania.
Nurses are Addressing Today’s Top Health Challenges
Caring for a growing aging population and the chronic care management that comes with it, addressing mental health issues (including addiction) and creating new ways to improve population health are some of the most perplexing health challenges today.
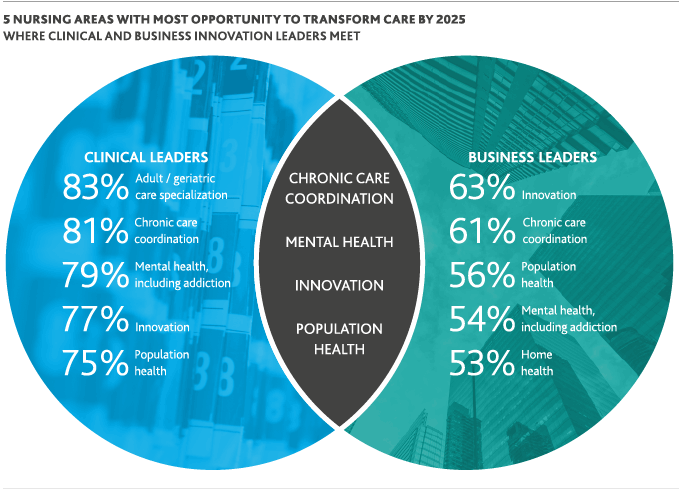
By 2025, clinical and business leaders agree that nurses have the most opportunity to transform and improve care in these critical areas.
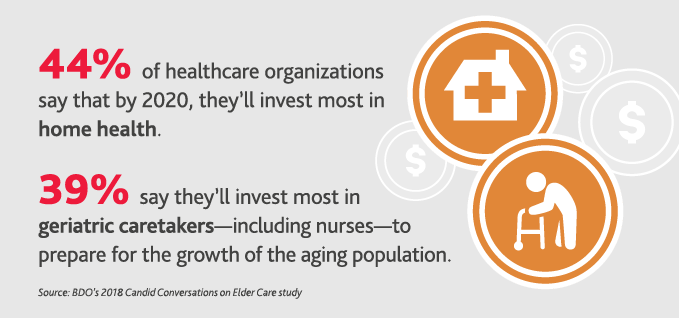
Nurses’ direct patient access and ability to develop patient-centered care solutions has made them natural leaders in addressing some of the most perplexing health challenges in history. That’s especially true when it comes to creating innovative senior care and chronic care coordination models—in a time when care is moving away from the hospital and into the home and community.
People tend to focus on nurses in hospitals, but that’s not the only place nurses exist, Clipper says. They’re serving across the community—coordinating care across a variety of modalities.
“We as nurses have a tremendous amount to offer in terms of input, feedback and thought leadership around not only the development of processes, systems and devices, but also in anticipating a lot of issues that can arise in patient care, including family dynamics,” she said.
One example is through nurses’ role building and leading the coordination of the Programs of All-Inclusive Care for the Elderly (PACE), which originated in San Francisco as a way to care for frail and elderly patients while still keeping them actively engaged in the community.
Through an adult day health center and supported by an interdisciplinary team—often led and coordinated by nurses of various practice levels—PACE provides preventive, primary, acute, behavioral and long-term care services for people 55 and older, most of whom are eligible for both Medicare and Medicaid.
PACE benefits go beyond traditional care to also include meals, nutritional counseling and social work counseling. In New York state, the quality of health for PACE beneficiaries is about twice as high as other managed long-term care participants. In California, in addition to better patient outcomes, PACE programs have also created at least 31 percent cost savings for the dual-eligible population compared to facilities-based care models.
“In a PACE model we led at Penn Nursing, nurse practitioners served both as primary care providers and care coordinators,” Villarruel said. “We were able to cost-effectively provide care and also coordinate services by attending to issues in the home, providing transportation and overseeing effective medication management.”
The Role of Design Thinking in Producing Greater ROI
Bowles’ research into what was driving high elderly patient readmissions in hospitals, which ultimately turned into a software solution and then a company, is an example of how nurses use research and technology to solve important healthcare issues.
In fact, both clinical and broader business leaders say such skills, paired with coordinating the interface of clinical innovation with technology, will be among the most valuable for nurse innovators by 2025.
Design thinking and the interface of clinical innovation with technology are key to developing, testing and evaluating new solutions across the health system—for those solutions to have any chance of success. In healthcare, this means taking an empathy, human-centered approach to solve for unmet patient needs with the goal being the triple aim of health: better care at higher quality and lower costs.
The American Academy of Nursing’s Edge Runner initiative, which recognizes nurse-designed models of care and interventions that achieve the triple aim of health—underlines the impact of encouraging this type of innovation.
Previous Edge Runners have included a nurse-managed interdisciplinary counseling network bringing behavioral health services to public housing residents and a nurse-designed multidisciplinary intervention developed and tested to reduce health disparities among the elderly—with the goal of helping them age at home.

Nursing a System-Wide Change in Mindset
Nurses have long been chief innovators. The health system just hasn’t capitalized on them yet.
Now, healthcare—one of the last big industries to think about innovation in a different way—doesn’t have a choice.
“Urgent health issues, new tech-enabled solutions, consumer demands, a mounting workforce shortage and the move to a value-based reimbursement model are forcing the industry to change its mindset,” Villarruel says.
At the same time, she adds, a new generation of nurses—born during the era of tech-driven innovation—is entering the workforce, driving a greater sense of entrepreneurship and creative spirit in the field of nursing.
Health stakeholders—providers, business leaders, regulators and governing bodies alike—can no longer relegate nurses to behind the scenes. Their ability to thrive amid the new consumer-driven health system depends on nurses having a seat at the table from the beginning and extending it to the leadership level.
To get there, health systems and businesses must:
- Remove barriers at the institutional, reimbursement, regulatory and policy levels that discourage nurses from practicing to their full scope, which 91 percent of clinical leaders say will be the most important area of nursing innovation for health organizations to invest in by 2025.
- Teach and support rigorous approaches to nursing innovation, which include design thinking and entrepreneurship skills in both academic and healthcare settings.
- Create organizational structures and incentives for interdisciplinary innovation teams to improve care.
- Elevate at least one nursing leader to the C-suite of every clinical and broader health business.
Clinical and business leaders alike have a direct stake in—and clear path for—doing so.
A system-wide shift in mindset, done right, would provide endless leadership opportunities for nurses to improve health outcomes.
Nurses are innovators. They are integral to creating patient-centered health solutions and uniquely positioned to address pressing health issues.
And sometimes, as Bowles proved, some of the best innovations start with just a simple question.
Are you ready to transform healthcare? Nurse innovators can lead the way.
SHARE